Dr Christin Eltze and Nicola Barnes, GOSH
Disclosures
- CE was PI for studies sponsored by GW Pharma
- CE has contributed to and chaired sponsored educational events
activities by GW Pharma and Nutricia (fees to departmental funds)

Tom
Syndrome diagnosis: Lennox –Gastaut Syndrome
- Birth history: uncomplicated (term NVD)
- Seizure onset: age 4 m → infantile spasms (responsive to VBT + Prednisolone)
- Seizure recurrence age 15 m → multiple seizure types (epileptic spasms, tonic sz drop sz)
- Evolution with global delay and profound intellectual difficulties, drug resistant epilepsy
- @ age 3 years:
- presurgical evaluation (CESS) – MRI: FCD right frontal lobe, ictal EEG (spasms)
variable lateralisation, subclinical seizures with onset either hemisphere - Pre-surgical counselling: 50 % chance of seizure freedom
- Right frontal lobe resection ( histology non-diagnostic )
- presurgical evaluation (CESS) – MRI: FCD right frontal lobe, ictal EEG (spasms)
- Seizure free for 3 months post surgery – then recurrence (multiple sz types incl drop
seizures) - VNS implanted age 6 years → no benefit in sz reduction
Tom – Progress – age 10 years
- Impaired mobility (unsteady gait – frequent drop seizures, required wheelchair)
- Communication: single words and gestures.
- Generally ‘happy’ but – Behaviour at times challenging:
- self-induced vomiting; episodes of screaming and
aggressive behaviour (pinching), Spitting
- self-induced vomiting; episodes of screaming and
- ASMs: valproate and clobazam
- Referred to back to CESS –
- underwent Corpus Callosotomy
Tom – post- Corpus Callosotomy
- Seizure free initially → more alert & socially engaging
- Mobility improved – walking independently at home
- 4 weeks post-op: refusal to eat and drink, non-compliance with ASMs
- Seizure recurrence (nocturnal seizures ) – hospital admission
- Required – feeding support with NG-tube and then gastrostomy
- 4 months post-op: increase of tonic seizures (nocturnal) + atypical absences
- Behavioural deterioration:
- aggressive behaviour, self-harming (head banging)
- Brain MRI – postoperative changes only, CC – complete; EEG – confirmed – not in
NCSE - Around the time underwent dental treatment under GA
- Behavioural deterioration:
Reasons for behaviour change, How we can support
- Prior to CAHMS referral all medical reasons for distress ruled out
- Have we woken up the child , now see true personality ????
Behavioural outcomes after Corpus Callosotomy
- Little information in literature
- Sharawat e al 2021, Child’s Nervous System (2021) 37:2557–2566 Efficacy and safety of CC and KD in LGS
- CC: 23 studies (436 patients)
- Average age at CC was 11.3 ±7.8 years, and the average time from seizure onset to CC was 8.6±6.9 years
- Average follow up 43.2±29.7 months.
- Seizure free: 40.78% (95%CI—28.24–53.33%); ≥ 50 % sz reduction 85% (anterior CC in 177/436)
- Only 5 studies assessed cognition and behaviour
- Improvement in behaviour and communication reported in 69%
Behavioural outcomes after Corpus Callosotomy
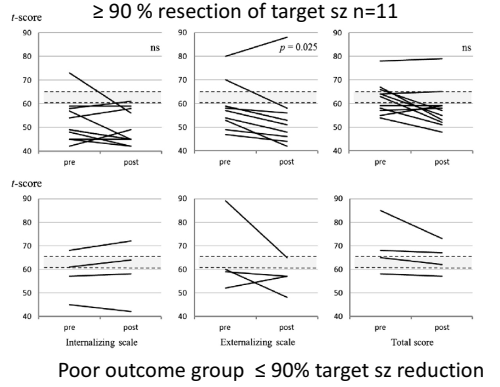
- Yonekawa et al, Epilepsy & Behaviour 22
(2011) 697–704 - N=15 retrospective (age 3.1-17.9 years)- target seizures – drop attacks (mostly LGS)
- Assessed with Child Behaviour Checklist :
- pre- and postoperative Attention Problems scores
showed no statistical differences between seizure
outcome groups - decrease in Externalizing scores for the patients
with a favourable outcome.
Lea, right handed, referred age 13 years
BMI > 99.6th centile
- Birth History: uncomplicated (term, NVD ); Early development – normal
- Seizure onset: age 2.5 years, prolonged left focal motor (25 minute duration)
- Focal seizures: aura: “stomach ache” evolving to bilateral tonic clonic seizures
- Drug resistant (failed 3 ASMs incl Levetiracetam not tolerated (aggressive behaviour)
- Learning difficulties – attends special school (does not like school)
- Behaviour: no behavioural concern, but peer-relationship difficulties – no friends
- Referred to CESS age 14 years, local brain MRI report 4– lesion negative (degraded by movement artefacts)
- Optimised MR imaging: right temporal lobe incl hippocampus/amygdala decreased grey/white differentiation,
- FDG-PET: right temporal hypometabolism
- VT-EEG : sz semiology – right mesial temporal onset, fear, preserved speech
- Neuropsychology: weakness in language , memory difficulties , ASD assessment recommended
- @ Age 16year 9 months: right anterolateral temporal lobectomy + amygdalohippocampectomy• (histology hippocampal sclerosis)
Low mood on discharge home
- Recovered well from surgery – discharged her on day 4
- Some anxiety observed before going home, reassurance given
- Post op call day 10: low appetite, refusing to leave bedroom , general lethargy, reporting abdominal aura but no sz
- 2 week post op: frequent calls from family, she was withdrawing from social media, crying +++ with one event of unresponsiveness, not typical of pre op events
- Review at GOSH for wound review – panic attack once home requiring local hospital assessment
- 4 weeks post op: psychiatrist review, low mood, no appetite, tearful, struggling to sleep , poor energy and no motivation. Was only settled if brought by father to GOSH reception to sit for a few hours every day and wished to be readmitted to hospital
Assessment and support
- Impression:
- Post-operative low mood, possibly adjustment reaction with generalised anxiety and a panic attack. This seems to be related to concerns about her feeling safe (on the ward) and some worries about her physical health (auras, pain and anxiety around seizures).
- Unable to facilitate readmission to ward, distraction techniques to encourage returning to usual activities she enjoys, cooking, TikTok
- https://www.nhs.uk/mental-health/children-and-young-adults/advice-for-parents/anxietydisorders-in-children/
- https://www.childline.org.uk/toolbox/calm-zone/
- https://hampshirecamhs.nhs.uk/wp-content/uploads/2018/03/Self-help-Workbook-Children-
1.pdf - Promotion of sleep hygiene
- Phased return to college
- Local CAHMS referral : sertraline prescribed, diagnosis of depression
Now
- 18 years old: continues on topiramate and sertraline
- Post op EEG captured ongoing abdominal pain, staring reduced responsiveness: not epileptic
- No seizures or aura reported since May 2024
- Dad reports that her mood is much better on sertraline
- She comes out of her room and mixes with the family and siblings
- She still can have low mood and can cry a lot. She can also get angry quickly, but laughs too
- There is ongoing CAMHS input
- She is happy she has lost weight
Psychiatric outcomes after temporal lobe surgery
De novo onset Depression
- Hue et al. Epilepsy & Behavior 134 (2022) 108853, Systematic review
- 18 studies, incl. patients > 18 y, patient numbers 49-230
- Variable assessment and measures, follow up 3m-9y
- Incidence 0 – 38% (many studies reporting improvement)
- Most within first year after surgery
- Risk factors (not primary aim)
- Pre-op: Pre-existing diagnosis + FH
- Post-op: family dynamics, patient adjustment, seizure control
Comorbid psychiatric disorder
- Ploesser et al, Epilepsy Research 189 (2023), Systematic review and meta-analysis
- 10 studies, children (1) + adults (8), both (1)
- Participants 22-115 (total 496)
- Follow up mostly 2 years (range: 1m-30y)
- Wide range of results
- Overall 43% improvement
- 33% worsening (adults 19-21%, Children 7-36%)
Do behavior and emotions improve after pediatric epilepsy surgery? A systematic review
C Reilly et al (Epilepsia. 2019;60:885–897.)
- 15 studies included (mostly High Income Countries)
- 12 of 15 TLEs surgery, ample size 28-100, 4/15 had control group
- 12/15 used standardised tools (CBCL, SDQ)
- Quality: 5/15 – moderate, 10/ 15 weak
- No study noted deterioration of behavior
- Studies using DSM – no significant change of children diagnosed at baseline and follow up (resolution of diagnosis in 21 and in 16 new diagnoses)
- Better seizure control associated with improvement
Pre surgical assessment
- CESS pathway allows neuropsychology testing of cognition, memory and language
- Neuropsychiatry assessment of mood of family, expectations for surgery, mood, may ask local CAHMS for involvement to support further diagnosis assessment of ASD, ADHD
Self injurious behaviour following epilepsy surgery
- SIB defined as self inflicted non accidental acts causing damage or destruction of body tissue, carried out without suicidal ideation or intent: self biting , self hitting , teeth grinding , object finger in cavities and hair pulling
- Assessment: psychiatric history , social needs and risk assessment
- Rule out medical causes , depression and ADHD, hyperactivity, impulsivity
- SIB can be chronic or refractory, premise for behaviour can be maintained by socially medicated reinforcement i.e. acquisition of instrumental/communicative functions, or alternately by automatic reinforcement, i.e. that there is a sensory seeking component. There is always a reason for challenging behaviour. It may not be easy to see at first. It is the child’s best attempt at telling you something.
Interventions
- ADHD, stimulant medication is generally safe and effective in children with epilepsy
- Positive Behavioural Support (PBS) patient centred, individualised approach, MDT support essential
- Functional Assessment: Aim to identify events that typically precede and follow episodes of self injury in order to form a hypothesis regarding factors eliciting and maintaining the behaviour. Use of an Antecedent–Behaviour–Consequence (ABC) checklist.
- Intervention
- Short term Non Contingent reinforcement
- Long term Implement a PBS traffic light system
- Green, keep child in green zone when behaviour is regulated, simple communication, positive reinforcement, set boundaries with PECS, visual planners, routine and structure
- Amber, recognise early warning signs, give the child what they want, divert or distract, do not respond if safe to do so, stay calm
- Red, behaviour is happening, divert, distract, low arousal approach, calm, regulate breathing, personal space
Pharmacological Management (Claire Eccles)
- Pharmacological Management- Consider STOMP/STAMP. Limited meta-analysis evidence for both antipsychotics or ASM and SIB unlikely to respond. Review NICE guidance.
- The guidance is clear that antipsychotic medication should only be used for challenging behaviour if:
- Psychological or other interventions alone do not reduce the challenging behaviour within an agreed time, or
- Treatment for any mental or physical health problem has not led to a reduction in the behaviour, or
- The risk to the person or others is severe (for example because of harming others or self-injury).
- General principles:
- Identify target behaviour, Start low and go slow (increased risk of EPSEs and NMS), Regular review after 3-4 weeks, Stop medication if no response in 6 weeks.
- Risperidone is licenced for short-term use (up to 6-10 weeks) for persistent aggression.
References
- Yates, TM (2004) The developmental psychopathology of self-injurious behavior: compensatory regulation in posttraumatic adaptation. Clinical Psychology Review, 24: 35–74.10.1016/j.cpr.2003.10.001
- Biswas A, Gumber R, Furniss F. Management of self-injurious behaviour, reducing restrictive interventions and predictors of positive outcome in intellectual disability and/or autism. BJPsych Advances.2023;29(5):337-341. doi:10.1192/bja.2022.49
- NICE Guidance [NG11] Overview | Challenging behaviour and learning disabilities: prevention and interventions for people with learning disabilities whose behaviour challenges | Guidance | NICE